
The Sentrii Process
Boost your financial stability by streamlining your billing processes and reducing claim denials, all while providing top-notch care to your patients!
With the Sentrii Revenue Care System, you'll gain access to
valuable insights and dedicated support to help you maximize reimbursements and ensure your practice thrives...
To Get the Results You Need, Consider Our Process...
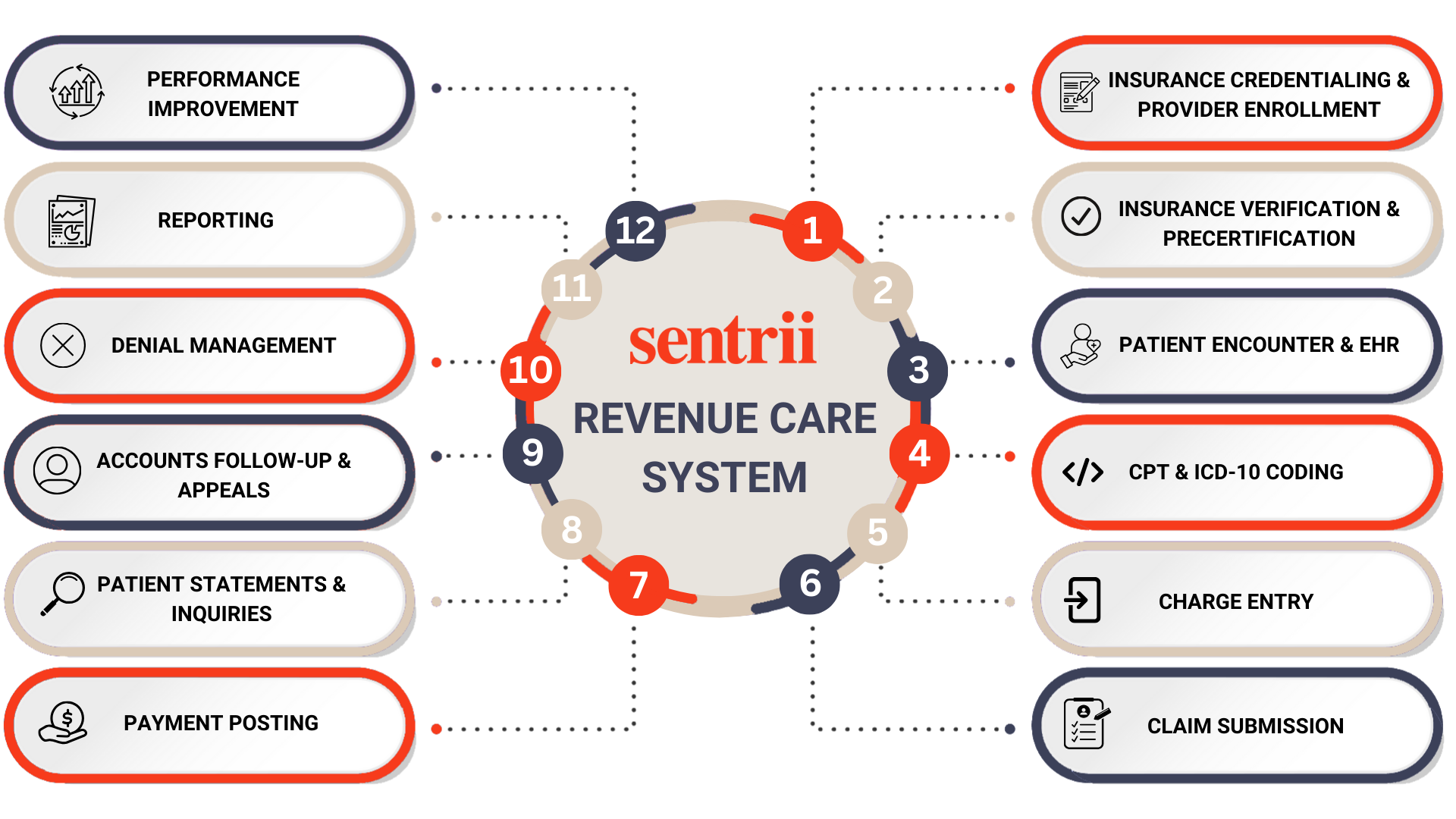
We streamline every aspect of the Revenue Cycle Management (RCM) process to ensure that healthcare providers maximize revenue, reduce inefficiencies, and eliminate costly errors. This visual representation highlights the 12 key steps in the medical billing lifecycle that Sentrii expertly manages.
Sentrii's Revenue Care System Explained
Sentrii's Revenue Care System is meticulously designed to simplify processes, maximize profitability, and enhance customer satisfaction. Our approach is structured around twelve essential steps, each crafted to address specific aspects of revenue management. These steps promote transparency and efficiency while ensuring continuous improvement across your practice!
INSURANCE CREDENTIALING & PROVIDER ENROLLMENT
- Management of payer applications and compliance.
- Simplifying the enrollment process to allow focus on patient care.
INSURANCE VERIFICATION & PRECERTIFICATION
- Validation and correction of insurance information.
- Evaluation of self-pay patients for alternative coverage options.
PATIENT ENCOUNTER & EHR
- Integration with electronic health records to ensure accurate documentation.
- Streamlining documentation processes to minimize errors
CPT & ICD-10 CODING
- Compliance and revenue maximization support through certified coding expertise.
- Comprehensive service reviews to identify areas for improvement.
CHARGE ENTRY
- Efficient charge entry processes with thorough reconciliations.
- Ensuring alignment between charges and original reports for billing integrity.
CLAIM SUBMISSION
- Quality control processes for claims before submission.
- Review for accuracy in demographics, coding, and compliance.
PAYMENT POSTING
- Electronic processing of payments with minimal fees.
- Tracking of financial transactions via reports.
PATIENT STATEMENTS & INQUIRIES
- Sending reminders for payment and managing outstanding balances.
- Coordination with collection agencies as needed.
ACCOUNTS FOLLOW-UP & APPEALS
- Analysis and appeal of denied or underpaid claims.
- Proactive approach to resolving claims efficiently.
DENIAL MANAGEMENT
- Root cause analysis of denials and implementation of process improvements.
- Use of data analytics to track and reduce denial trends.
REPORTING
- Provision of financial oversight through accounting and management reports.
- Regular meetings to align on goals and optimize processes.
PERFORMANCE IMPROVEMENT
- Continuous monitoring and refinement of processes.
- Collaboration with clients on operational enhancements for efficiency and financial performance.
Benefits of Using The Sentrii Revenue Care System
Increasing Revenue Without Extra Effort
By reducing billing inefficiencies and improving reimbursement rates, Sentrii helps you generate more revenue without needing to add extra staff or take on additional patient appointments.Reducing Denials and Rejections
Claims are validated before submission, ensuring accuracy and prompt follow-up on issues. This approach improves claim approval rates, minimizes costly rework, and frees up valuable time for your team.Enhancing Patient Satisfaction
Sentrii helps create a positive experience for patients by making billing efficient and transparent. This leads to higher satisfaction, fewer billing-related disputes, and improved patient loyalty.Streamlining Communication
Sentrii integrates seamlessly with your existing systems, enhancing communication between staff and payers. This reduces confusion and accelerates your billing process.Here are Some Frequently Asked Questions Our Staff Gets...
Is there a long-term contract?
We offer a 90-day termination clause in all our contracts, allowing flexibility for our clients. While the traditional approach was to use long-term contracts to cover ramp-up costs, we now structure those costs based on the specific work needed, eliminating the need for long-term commitments
How soon can I get started?
If there are no termination clauses to navigate and you can facilitate administrative control, we can get started right away. Our team is prepared to ensure a smooth transition with minimal disruption to your operations
Is it painful to transition to a new billing company?
Transitioning to a new billing company can be challenging, but a lockbox can help streamline the process by consolidating payments from multiple sources into a single location. While there may still be some initial setup and coordination required, using a lockbox minimizes payment disruptions and simplifies cash flow management, making the transition smoother and less painful. Proper planning and communication with payers can further reduce potential issues
How long will it take for me to see improvements?
Our reports are reliable, but the timeline for seeing improvements depends on several factors, including the quality of prior data and the specific changes implemented. While an apples-to-apples comparison is ideal, we often inherit incomplete or inconsistent data, requiring time to normalize and establish accurate benchmarks. Typically, meaningful trends become apparent within a few billing cycles
Can you work with my current staff?
We always strive to incorporate existing staff whenever possible, as long as they are willing and able to contribute effectively. We understand that external billing vendors can sometimes be met with hesitation, but our goal is to work collaboratively and ensure a smooth process while valuing the expertise already in place. Finding good talent is challenging, so we’re happy to work with your current staff to maximize efficiency and success
How much do you charge?
Our pricing is typically based on a percentage of collections, which varies depending on your practice's volume and specialty. Patient billing, including mailed statements, text, and email bills, is charged separately at cost, with digital options often being more affordable. Provider credentialing and enrollment are offered à la carte, and we also provide a wide range of optional services, from appointment reminders and eligibility checks to consulting and utilization reviews. For smaller practices, we have a minimum fee designed to be affordable. Let’s discuss your specific needs so we can provide a tailored quote